Therapy, Plans and Assessments- Frequently Asked Questions
The team at Lit Therapy are often asked a lot of questions, which we love! We have compiled a list of the questions most frequently asked in one easy spot for you below:
What is the difference between a Psychologist, a Provisional Psychologist, a Clinical Psychologist and a Psychiatrist?
A Psychologist is someone who has undergone 6 years of training in the field of psychology. This training might include the whole 6 years at university, or a combination of university study and an internship. The 4+2 pathway to becoming a psychologist includes 4yrs at university and a 2yr internship under frequent supervision. The 5+1 pathway to becoming a psychologist consists of 5yrs at university and a 1yr internship under frequent supervision. Once the internship is completed there is a National Psychology Exam to pass before being able to apply for general registration from Australian Health Practitioner Regulation Agency (AHPRA) as a registered Psychologist. Psychologists can support you to understand and manage your mental health symptoms, concerns and conditions or any general worries and stressors. They can also help you to understand behaviours and how you might relate to others and your environment, and much more.
A Provisional Psychologist is someone who has completed either 4 or 5 years of study at university in the field of Psychology and is currently undertaking their 1 or 2 year internship. Provisional Psychologists are still required to be registered with AHRPA and undergo frequent supervision sessions from an AHPRA Board Approved Supervisor to assess their therapy knowledge and intervention skills. Provisional Psychologists will need to sit and pass the National Psychology Exam before being eligible to apply to AHPRA for general registration as a psychologist. Provisional Psychologists are able to support you to understand and manage your mental health symptoms, concerns and conditions or any general worries and stressors. They can also help you to understand behaviours and how you might relate to others and your environment.
A Clinical Psychologist is someone who has completed their 6 years of training and gained their general registration as a Psychologist and has gone on to complete further studies in either a Masters or Doctorate degree in Psychology and achieved endorsement from AHPRA in the area of Clinical Psychology. They have gained further knowledge and skills in assessing, diagnosing and managing mental health symptoms and conditions on top of all that is previously mentioned that a Psychologist can do.
A Psychiatrist is someone who has studied medicine at university and is a qualified practicing medical doctor and gone on to further specialised study in psychiatry which includes psychology and mental health. A psychiatrist is someone who can assess, diagnose and treat mental health concerns and conditions. They can prescribe medication for managing mental health conditions whereas Psychologists and Clinical Psychologists cannot prescribe medication. Often times, an appointment with a Psychiatrist can feel more like a consult with assessment and diagnostic discussions with a management plan (which might include to see a psychologist and take medication) compared to a lengthier talk-therapy appointment with a Psychologist. A referral from your GP is often required to see a Psychiatrist and this referral may also entitle you to a Medicare rebate.
What is a Mental Health Care Plan?
A mental health care plan (MHCP) is a plan written up by your regular GP which enables you to receive rebates from Medicare to reduce the overall cost of up to 10 sessions with a Psychologist. The MHCP itself does not expire however you can only access Medicare rebates for up to 10 sessions per calendar year.
Once you have completed 6 six sessions using your MHCP and you would like to continue therapy, your psychologist will write to your referring GP letting them know you have had 6 sessions and would like to access the remaining 4 sessions. After 6 sessions you will need to go back to your GP for a MHCP review for them to enable access to your remaining 4 sessions.
A MHCP does not entitle you to free sessions. You pay the upfront cost of your psychologists fees and our admin team submit a claim to Medicare on your behalf so you receive a reimbursement of part of that upfront payment, leaving you with a reduced out of pocket cost.
Medicare unfortunately do not provide rebates for appointments with a Provisional Psychologist. Because of this, Lit Therapy have agreed to reduce the upfront cost of appointments with their Provisional Psychologists which leaves you out of pocket the same amount as it would if you were accessing rebated sessions with a registered Psychologist.
You do not need a MHCP to access psychology services – though having one can provide your psychologist with background information; and allow you to receive rebates for up to 10 sessions per calendar year making your therapy journey that bit more affordable.
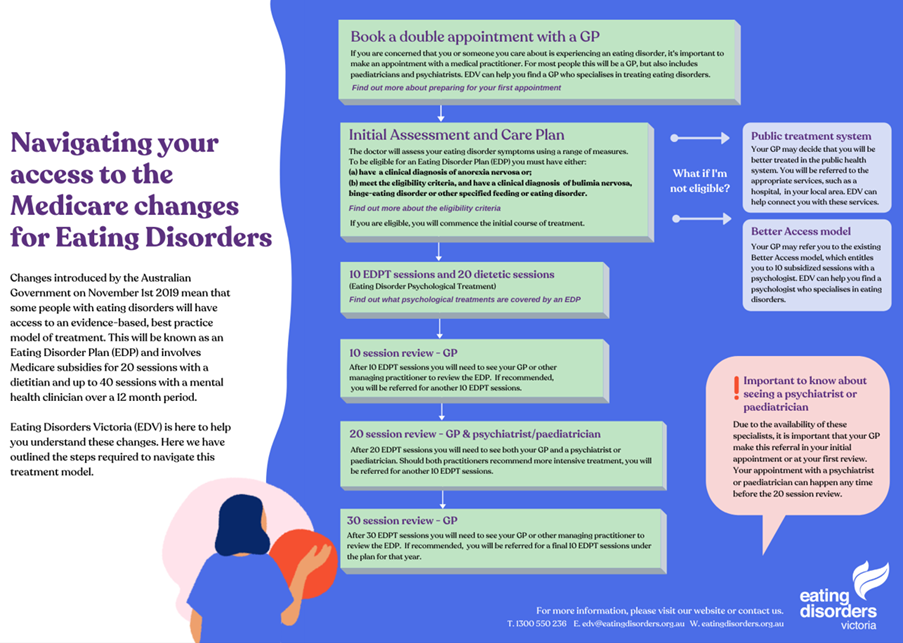
What is an Eating Disorder Plan?
Though we know recovering from an eating disorder is possible, we also know eating disorders have the highest mortality rate of all mental health conditions. Due to the nature of recovery, it can be a hard and lengthy process. An Eating Disorder Plan (EDP) is a government initiative to provide those struggling with an eating disorder access to more affordable treatment as they have recognised the severity of the challenge that recovery can be. An EDP essentially allows you to receive Medicare rebates for up to 20 sessions with a Dietitian and up to 40 sessions with a Psychologist over a 12month period (from the date of your plan). You can discuss your eligibility for an EDP with your GP and or psychologist, though EDPs are written by your GP – you will need to book a double appointment. During your treatment using an EDP you will need to be reviewed periodically by your GP and Psychiatrist/Paediatrician (depending on your age) for continued access to rebatable sessions on your EDP.
EDP Reviews- When to see your GP and Psychiatrist/Paediatrician?
Essentially you will need to be reviewed by your GP at the end of every 10 sessions with your psychologist (to access the next 10 sessions). At the half way mark- after your 20th session with psychologist you will need to be reviewed by your Psychiatrist or Paediatrician (to access the next 20 sessions of your EDP).
How long will I be in therapy for and how often should I come?
Frequency of sessions can really depend on a few things - your reasons for coming to therapy, your motivation, your schedule, your budget, clinicians recommendations and availability are all things to consider when booking in your sessions.
Often weekly to fortnightly sessions are recommended initially to help you and your clinician establish a therapeutic relationship, understand you and your therapy goals, come up with a therapy plan and make progress. You might start with weekly appointments and over time you might move to fortnightly and then to monthly appointments. This frequency might move up and down as your needs and availability change.
How long you might need to attend appointments for also depends on how complex your needs are and how you’re able to respond to therapy. This amount of time will vary from person to person and can be discussed with your clinician. Even when you make progress and achieve your therapy goals sometimes it is helpful to reduce your frequency and still come in for maintenance work and a therapeutic tune up as required to help you keep up your progress.
If finances are impacting how often you can see your clinician, have a chat with your GP to see if you meet eligibility for a mental health care plan or chronic disease management plan to be able to access Medicare rebates on some of your psychology sessions to reduce your out of pocket expenses.
Sometimes clinicians calendars can get quite busy so it can be useful to book ahead of time and reschedule or cancel as required, so then you know you’re in! Just be mindful of your providers cancellation policy and fees (click here to see Lit Therapy’s cancellation policy).
Ultimately though, it is up to you how often you book in for and for how long. Your clinician will get to know you, your concerns and will have a professional recommendation as to what your therapy plan might look like for you. If you can’t come as often as you would like to due to work, school, mood, dollars or other factors, your clinician can alter the therapy plan to meet you where you’re at with what frequency you can manage.
How you can make the most of your therapy sessions
While there is no wrong way to do therapy there are some things you can do to get the most out of your appointments:
· Preparing for sessions – this can include: putting your next appointment in your calendar so you can be reminded you have an appointment coming up so you can plan for it in your schedule and so you don’t forget to show up. It might be having a think about what you would like to talk about in your session or what you might like to ask your clinician. It can be hard to remember a list of things you come up with so you can definitely write it all down and bring your list with you.
· Take notes – sometimes its hard to remember all the stuff you discuss with your clinician so you can definitely take notes during your session. Often progress is made outside of your therapy sessions so taking notes can help you remember what you’re working on between sessions.
· Setting goals – You might know exactly what you want out of therapy and sometimes establishing your therapy goals may come from discussions with your therapist. Being an active participant in the goal setting process can be valuable for you and your therapist to know how to proceed together and ensure you are getting what you want and need out of therapy.
· Monitor your progress – how do you know if you’re making progress or not? Sometimes your clinician might notice changes in how you present in sessions over time and reflect this with you, or we might ask you to track particular data over the course of your therapy between sessions to know if there are any changes over time. Or we may ask you to complete forms in session or between sessions. It will be helpful to let your therapist know what is getting in the way of any progress. This progress data can help your clinician to know when or if they need to alter their therapy plan for you.
· Homework – Sometimes your clinician might want to set you a task to complete between sessions, whether that be a worksheet, tracking data, trying something new- whatever it is, your clinician should be explaining what it is, how to do it, why they’d like you to do it, and go through any problem solving aspects to be able to complete the task. There will always be a valuable therapeutic reason for requesting the task to be completed. Sometimes attempting the homework might go very well and sometimes it might turn out you’re not yet able to complete the task for a whole range of reasons and that’s ok too. Having a go is all we ask and discussing outcomes of the task can help guide your therapy process. If you’re ever not sure what is expected from any set tasks you can always ask and discuss with your therapist. If you ever feel you’re not ready or able to complete a task you can let your therapist know this too.
· Talk to your therapist – let us know what’s helpful for you in sessions and what is not helpful for you; let us know about what might be in the way of making progress; and ask questions.
How to find the right therapist?
One of the single most beneficial factors to anyone’s therapeutic outcome is how well you gel with your therapist so it makes sense you want to find the right one for you. A lot of psychology practices have online profiles of their therapy team on their website- have a read of some online profiles to see if there are any key words that might match your values and needs from a psychologist. This might give you a starting point as to who you might like to work with.
You can always ask a clinician about their experience and qualifications to see if they have the relevant skills to be able to help you. Ideally though, its about how you feel sitting in a room with your therapist. Do you feel comfortable in their presence? Do you feel able to speak openly and free from judgement to your therapist? Do you trust they have the right skills to support you and meet your needs? Sometimes it can take a few sessions to work this out but if you answered no to any of these questions you can let your therapist know so you can both workshop how to improve your therapeutic relationship moving forward. Alternatively you can shop around til you find someone more fitting for you. Your therapist won’t be offended if you switch clinicians, we understand its part of the process for you to find the right person for you. You should never stick with a therapist you are not comfortable with as this can limit how open and honest you are which might then limit your progress- it doesn’t mean they are a bad therapist. Therapists are also human and deliver their knowledge and skills with their personalities and just like any relationship you have – its either a match you can work with or it isn’t. If it’s a match – great! If not – do not let it stop you from accessing the support you need, try out the next one.
Once you find a therapist that feels comfortable for you its useful to keep seeing the same therapist for as long as is appropriate. This way, you will get to know how each other works and build a therapeutic relationship and a therapy plan for you to work towards. The stronger your therapeutic relationship, the more likely you are to go beyond surface level conversation which is useful to get to in order to make progress. It won’t be useful to chop and change therapists if you can help it as you will likely find you’re spending time on repeating things or may even become confused if the therapists are using different intervention skills to support you. Your therapist also gets know you and the way you respond to therapy and can use this information to guide how they formulate and deliver their plans for you.
Expectations for parents of a child in therapy:
Children and teens come with their own set of thoughts, feelings and behaviours they are learning to understand and manage as they grow and develop. This isn’t always an easy task for them as their bodies are changing, their physical needs change, and so can their environments. Young people often have stressors and worries relating to their friendships, their school work, their family, their health among other things and sometimes they can struggle with the juggle aswell. When your child is having trouble managing their thoughts, their feelings and their behaviours and this is impacting on their day to day lives and getting in the way of things they enjoy, or interrupting their usual sleeping and eating habits or causing them harm, it can be a good idea to seek support from a professional.
Depending on the age of your child, if they’re on the younger side, you might expect to be in the session with your child for most of your sessions so the therapist can support you to support your young person. If your child is a bit older, around 12 and up you might expect to come in for a session with your child for an introduction and set goals and expectations together with the therapist and after that therapy will likely be between the therapist and your child. Though if your child prefers you to be in the therapy room too then that will be supported until they feel comfortable for you to leave them to it.
As a parent it is not uncommon to feel left out if you’re out in the waiting room while your child is having their session no matter their age. Its pretty normal to want to know the ins and outs to know how to help your child with what they’re going through. This is where confidentiality and trusting in the process comes in. We want your child to feel safe in their sessions to talk about what is going on for them so we are best able to help them. You’re child’s sessions are confidential whether you’re in the room with them or waiting in the room. If the therapists disclose anything or everything that is discussed in the young persons session without their consent – even to parents - the young person often loses trust in their therapist (or therapy in general). It is important we maintain the childs trust so we are in a strong position to support your child which is the reason it might seem like we aren’t telling you everything.
If there is anything that we think you may be able to help your young person with between sessions ie any strategies to practice, we will let you know with your young persons consent. If your child discloses anything concerning to us that relates to their safety (or someone else’s), rest assured we will let you know in a timely manner and support you with this.
How you can support your young person in therapy:
· Ensure they are comfortable with the therapist they are seeing.
· Bring your young person to all their scheduled appointments.
· Listen to your child if they want to talk through what they have learned and talked about in their session.
· Trust in the process and show patience if they choose to not share what they are working on or talking about in their sessions.
· Where guided by your therapist, support your child with any therapy ‘homework’, model or remind your young person of the skills they can practice between sessions.
· Ask your child and their therapist how you can help so there are clear expectations of your role as a parent and how you can help your childs therapeutic process.
· If you’re separated from your childs other parent and are co-parenting in different environments- talk to your childs therapist for tips on how to navigate the level of involvement each parent has in your childs therapy process, as the tips will vary for different families.
Assessment Pathway for ADHD, Autism and learning disorders in Children, Teens and Adults
If you’ve noticed your child has challenges with their behaviours, their ability to learn or hold information and attention, or the way they relate to others and would like to have your child assessed for Attention deficit Hyperactivity Disorder (ADHD), Autism Spectrum Disorder (ASD) or a specific learning disorder such as Dyslexia, Dyscalculia, Dysgraphia, Visual Processing disorder and working memory concerns an assessment may be recommended.
Tips for your Assessment appointment:
· Have a chat with your childs school or daycare and see if they have noticed any of the concerns you have.
· See your Paediatrician and prepare for the appointment with your (and school/daycare) observations and a list of questions.
· In your appointment you can expect to be asked a series of questions about your child’s development from birth and they will likely request questionnaires to be completed by parents and your childs teacher as part of the assessment process. Your clinician will use this information to rule out other explanations for your or childs challenges in order to make their assessment and or diagnosis.
· Your clinician will recommend treatment strategies for your childs symptoms or diagnoses which may include medication and or seeing a Psychologist, Occupational Therapist, Speech Therapist, Physio, Tutor and/or other to facilitate and support you and your childs needs and progress.
· While Psychologists at Lit Therapy can conduct preliminary assessments and support you with management strategies associated with ADHD; ASD; and learning disorders we do not currently have psychologists who formally assess and diagnose ASD; ADHD; learning disorders. Feel free to ask us for a list of alternate providers who formally assess ASD; ADHD; and learning disorders.